The Human Immunodeficiency Virus (HIV)
Perhaps no disease is more strongly identified with the late twentieth century than acquired immunodeficiency syndrome, commonly known as AIDS. Yet, according to a 2004 United Nations report on the state of the global AIDS epidemic, the disease has not yet begun to reduce its grip on the world population despite the fact that AIDS does not generally receive the same amount of public attention as it once did. On the contrary, infections are on the rise in many countries, including high income nations such as the United States. In 2003, nearly five million people contracted the human immunodeficiency virus (HIV) that causes AIDS, the greatest number of new infections in a single year since AIDS was first officially recognized as a disease in 1981.
The virus responsible for HIV was first isolated in 1983 by Robert Gallo of the United States and French scientist Luc Montagnier. Since that time, a tremendous amount of research focusing upon the causative agent of AIDS has been carried out and much has been learned about the structure of the virus and its typical course of action. HIV is one of a group of atypical viruses called retroviruses that maintain their genetic information in the form of ribonucleic acid (RNA). Through the use of an enzyme known as reverse transcriptase, HIV and other retroviruses are capable of producing deoxyribonucleic acid (DNA) from RNA, whereas most cells carry out the opposite process, transcribing the genetic material of DNA into RNA. The activity of the enzyme enables the genetic information of HIV to become integrated permanently into the genome (chromosomes) of a host cell.
The primary hosts for HIV are the white blood cells variously called helper T lymphocytes, helper T cells, or CD4+ T cells. These cells are important components of the immune system that are normally responsible for activating the responses of many other immune cells. Helper T cells that become infected with HIV rapidly die. Soon after primary infection, the body is usually able to compensate for the loss of infected T cells by producing them in greater quantities, at which time individuals infected with HIV are asymptomatic. Over time, however, the virus becomes increasingly acute and there is a slow decline of helper T cells. Consequently, the number of helper T cells in the body (termed the CD4 count) is generally utilized to gauge the advance of the virus. A CD4 count of less than approximately 200 cells per microliter of blood may be accompanied by a variety of opportunistic infections and is considered the final stage of infection. The persistent barrage of such infections is what typically leads to the death of AIDS patients.
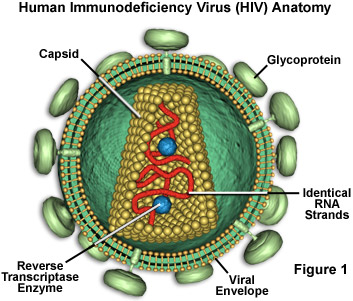
HIV is a relatively complex virus that is able to infect helper T cells chiefly due to a glycoprotein embedded in its envelope called gp120 (see Figure 1) that attaches to CD4, a protein found on the surfaces of the T cells. Entry of HIV into a host cell is also thought to involve a co-receptor on the cell surface, either CCR5 or CXCR4, which typically function as receptors of chemokines. The HIV virus envelope is a derivative of the plasma membrane of a host cell, obtained via budding. When HIV attempts to enter a cell, interactions between cell surface molecules and viral envelope proteins allow the envelope to fuse with the cell membrane. The envelope protein called gp41 is known to play an important role in this process.
In an infected cell, HIV undergoes reverse transcription, producing double-stranded DNA from its RNA with the help of reverse transcriptase, a specialized virus-specific enzyme that transcribes DNA from an RNA template. Once in DNA form, the genetic information of HIV is incorporated as a provirus with the host cell DNA. The proviral genome can subsequently be transcribed into viral RNA that functions as mRNA for translation into HIV proteins and as genomes for the subsequent generation of the virus. Capsids form around the viral genomes and proteins before they are budded from the cell membrane, further encapsulating the material into envelopes.
The replication process of HIV is associated with a very high mutation rate because reverse transcription does not allow for correction of errors in nucleotide incorporation. HIV evolves at rate a million times more rapid than the evolution of the human genome, making it extremely difficult for the immune system to recognize and effectively combat. For similar reasons, the development of drugs or vaccines for HIV is a complicated endeavor, the virus not only varying greatly from patient to patient, but even exhibiting significant genomic discrepancies in individuals. A cure for HIV continues to remain elusive, but significant advances have greatly improved the quality of care that patients can receive. Highly active antiretroviral therapy (HAART), which involves the use of multiple reverse transcriptase and protease inhibitors, has proved a highly beneficial form of treatment for many patients, but the cost of the therapy has prevented its widespread use in many parts of the world hardest hit by HIV and AIDS.
