|
The chemotherapy of bacterial infections dates back to 1935, when the synthetic group of drugs commonly known as sulfonamides, or sulfa drugs, was introduced. Examination of mortality rates in England and Wales from that time onwards indicates that these drugs reduced the mortality from hemolytic streptococcal infections (typified by puerperal fever), pneumonia, and cerebrospinal fever. Though often referred to as antibiotics due to their bacteria-fighting ability, sulfonamides are not derived from living organisms and should not, therefore, be classified as such according to traditional usage of the term. It was not until several years after sulfonamides became available that true antibiotics derived from, or produced by, fungi, bacteria, and other organisms, were added to the arsenal of medicinal weapons available for combating bacterial diseases.
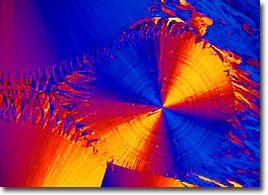
Erythromycin
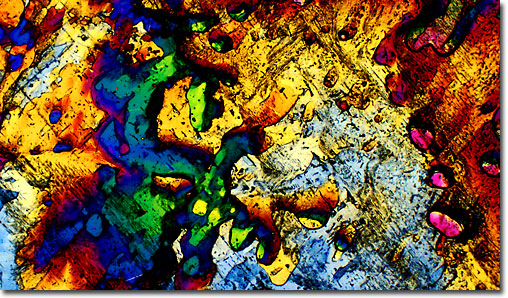
Penicillin, the first antibiotic ever discovered, helped revolutionize the medical field during the twentieth century. Knowledge of this important and powerful antibiotic began with Alexander Fleming, who in 1928 observed by chance that the growth of bacteria he was attempting to culture in his laboratory was inhibited by a contaminating mold (Penicillium). Fleming correctly deduced that the mold was producing a substance, which he termed penicillin, produced this unusual effect, but was unable to isolate the material. During World War II, an increased necessity for finding ways of treating infections suffered by wounded members of the military resulted in increased interest in penicillin research. The first to isolate and chemically characterize the substance were pathologist Howard Florey and biochemist Ernst Chain, whose achievements led to the ability of generating sizable quantities of the antibiotic, which quickly became a widespread form of medical treatment.
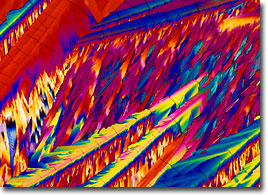
Clindamycin
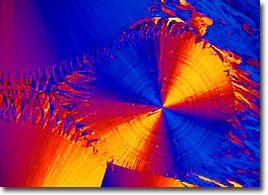
Today, there are hundreds of derivatives of penicillin that have been developed, including the semi-synthetic compound ampicillin that appears on the banner above, as well as a wide range of other antibiotics. Indeed, shortly after the introduction of penicillin to the world, René Dubos, an American scientist, found that a soil bacterium was able to render pneumococcus bacteria innocuous, and his further efforts revealed that a substance dubbed tyrothricin derived from the bacterium was actually able to combat an impressive array of infectious bacteria. Around the same time, American microbiologists Selman Waksman and Albert Schatz isolated streptomycin and a variety of other bacteria-fighting agents from the microbe Streptomyces griseus. These and additional antibiotics that have since been developed are responsible for saving innumerable lives and improving the quality of life for countless others.

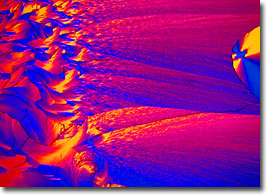
Amoxicillin
Antibiotics are not only utilized as a form of medical treatment for humans, however. The drugs are also frequently included in the diet of cattle and other farm animals. This controversial practice, which is often carried out even for healthy livestock, is intended to increase the weight of the animals, which correspondingly increases their economic value. For similar monetary reasons, antibiotics are also widely used to treat a number of plant diseases caused by bacterial infections, often enabling farmers to avoid significant crop losses. Yet, although utilization of antibiotics for such purposes may make short-term economic sense, many are skeptical and believe long-term concerns about the increasing immergence of antibiotic-resistant strains of bacteria, which common exposure to antibiotics promotes, should take precedence. For similar reasons, many in the scientific community also find the everyday use of antibiotic soaps and lotions that has arisen among the general public in recent years problematic.

Ofloxacin
The development of bacteria that are resistant to antibiotics essentially occurs due to the evolutionary process and natural selection. More precisely, when a group of bacteria are exposed to an antibiotic, only those that exhibit a certain trait or mutation can survive. These remaining bacteria reproduce and pass the same characteristic to their offspring, resulting in an entire generation of microbes that are resistant to that particular compound. Antibiotic-resistant bacteria were discovered as early as the 1960s, when strains of both pneumonia-causing pneumococcus and the Neisseria gonorrhoeae bacterium that is responsible for gonorrhea were discovered. Some of the other common bacteria that have since been found to be unaffected by antibiotics that were formerly effective in rendering them harmless include Salmonella, Streptococci, and Escherichia coli.
Chloromycetin
Many strains of bacteria have become, in fact, resistant to multiple antibiotics. These remarkable microorganisms are commonly referred to as "superbugs" due to the incredible difficulty in combating them. As more and more multiresistant bacteria evolve, the faster pharmaceutical companies must race to develop new antibiotics to fight them. If they are unable to meet the challenge, illnesses that came to be considered trifling occurrences in the twentieth century may once again become a cause for alarm.
|